Moles And Your Skin
There are several skin lesions that are very common and benign (non-cancerous). All of them are often called “moles” but include other conditions including cysts, warts, haemangiomas, freckles, skin tags, benign lentigines, lipomas and seborrheic keratoses. In this little exert we will try and explore the common lesions often seen, how to recognise them, what we can do about them and most importantly how to recognise a potentially cancerous mole.
Moles
Moles are growths on the skin that are usually brown or black. Moles can appear anywhere on the skin, alone or in groups. Moles typically start to appear in early childhood and during the first 25 years of a person’s life. It is normal to have between 10-40 moles by adulthood. However, this can vary from person to person, and they can start to appear later in life. Over time moles naturally change slowly. This does not indicate that they are necessarily cancerous. Typical changes over a long period include becoming raised and / or changing colour. Occasionally hairs can appear in a mole. Some moles may naturally disappear over a period of time.
The causes of moles are not uniform. In simple terms, they occur when cells in the skin grow in a cluster instead of being spread throughout the skin. These cells are called melanocytes (melanin – pigment forming cell), and they give the skin its natural colour. The greater the number of melanocytes, the darker the skin. Moles may darken after exposure to the sun, during the teenage years, and during pregnancy.
Types Of Moles
A nevus (pleural nevi) is a congenital mole of the skin and is present from birth. Congenital nevi occur in one in every hundred people and are marginally more likely to develop into melanoma (skin cancer) than are moles that appear after birth. A mole or freckle should be checked if it has a diameter of more than a quarter of an inch – often compared to being bigger than a pencil eraser. A mole should also always be checked if it shows any of the characteristics (ABCDE) of a melanoma (refer to the section on recognising a mole that is cancerous).
Dysplastic nevi are moles that are much less common. They generally tend to be larger than the average nevus (larger than a pencil eraser) and often irregular in shape. They can be uneven in colour with dark brown centres and lighter, uneven edges. These nevi are somewhat more likely to become a melanoma. Statistically, people who have 10 or more dysplastic nevi have a 12 times greater chance of developing melanoma (skin cancer). Anyone suspicious of a having one or more dysplastic mole(s) should have these checked by a doctor with an expertise in skins or a dermatologist.
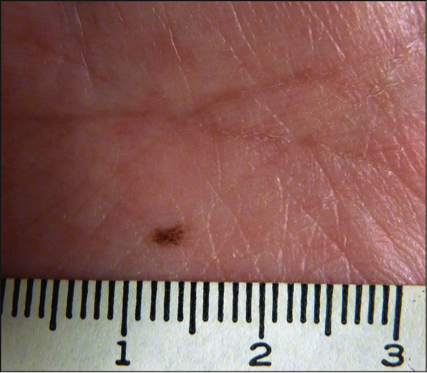
Congenital Nevus
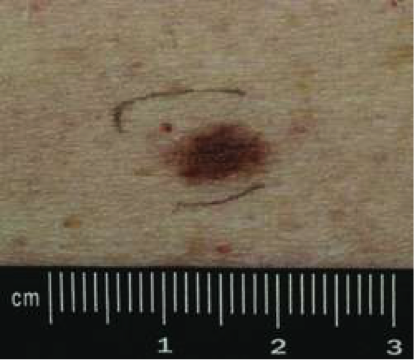
Dysplastic Nevus
Recognising A Mole That Is Cancerous
The majority of all moles are not dangerous or cancerous. Moles are more likely to be cancerous if they look different than other existing moles or those that first appear after the age of 25. If you notice changes in a mole’s colour, height, size, or shape, you should have a dermatologist or a doctor with skin expertise evaluate it. You also should have moles checked if they bleed, ooze, itch, or become tender or painful.
Examine your skin regularly with a mirror or ask someone to help you. Areas of the skin that are often exposed to the sun, such as the hands, arms, chest, neck, face, ears, legs, and back need extra attention. Taking pictures of your moles next to a ruler and comparing them over time can be an effective way of monitoring your moles. Moles that don’t change over time have little reason for concern. However, If you see any signs of changes in an existing mole, if you have a new mole (especially after the age of 25), or if you want a mole to be removed for cosmetic reasons, talk to your GP about being referred to a dermatologist or see a doctor with an expertise in skin.
There is a simple ABCDE to follow and consider when examining moles. If a mole displays any of the signs listed below, it is best checked immediately by a dermatologist or a doctor with expertise in skins as it could be cancerous.
- Asymmetry. One half of the mole does not match the other half.
- Border. The border or edges of the mole are ragged, blurred, or irregular.
- Colour. The colour of the mole is not the same throughout or has shades of tan, brown, black, blue, white, or red.
- Diameter. The diameter of a mole is larger than the eraser of a pencil (a quarter of an inch).
- Evolution (changing characteristics). The mole is changing in size, shape, or colour.
Treating Moles
If a doctor believes a mole may be sinister or needs further evaluation, they will arrange for a biopsy by shaving or cutting out the entire spot so that it can be examined under the microscope. This is a simple procedure and can be done under local anaesthetic. If the mole is found to be cancerous, the dermatologist will cut out the entire mole or scar from the biopsy site. They will cut out the entire area and a rim of normal skin around it, and the skin stitched back together again.
Other moles don’t necessarily require removal as far as they are regularly checked. A mole that is dysplastic or cosmetically unfavourably can be removed. There are many choices on how mole removal can be done. They could be excised (cut out) under a local anaesthetic with the area being stitched closed. If this is done professionally, the scar can be minimised. Other choices include being treated by less invasive options such as PlexR. The advantage of less invasive options (where applicable) is that it removes the risk of scarring, an important consideration for a potentially cosmetic procedure. The important thing is to speak to a doctor that is experienced and trained in all the options so that you can make the most appropriate and informed choice for your mole.
Client Before and After Example
Below are two examples of mole removal treatments performed on past clients at LasaDerm. Both examples are excisions where the mole has been cut out and stitched, and the stitches removed one week later.
Before

After

Before

After

